What is psoriasis?
Psoriasis is an immune-mediated disease (inflammation caused by the immune system)2. It’s a chronic condition that usually appears on the elbows, knees, scalp and lower back. However, it can appear anywhere on the body. It’s a long-lasting condition; for many, once it first occurs, they have it for the rest of their lives.

Causes & treatment
-
What causes psoriasis?
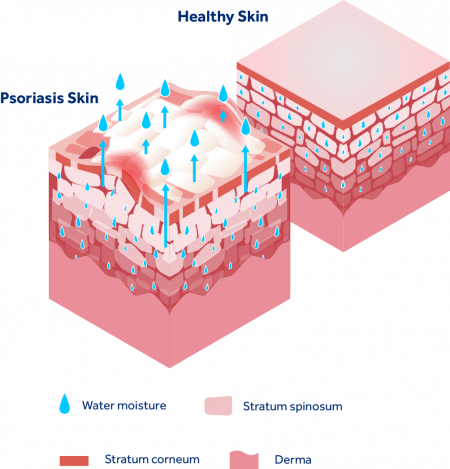
Psoriasis occurs when your skin’s cells multiply too fast, as the overactive immune system speeds up cell growth. Normally, the skin renews itself every 3 or 4 weeks. But, if you suffer from psoriasis, it happens every 3 to 7 days. This breaks down the protective skin barrier, allowing the escape of moisture and the build-up of thick, scaling skin.
-
What does psoriasis look like?
The condition can vary depending on skin types, and is characterised by:
- Raised plaques
- Red flaky skin
- Crusty patches
- Dry or cracked skin
- Thick, silvery scales
Many of those with psoriasis report that these patches can burn, itch or bleed. Other symptoms include thickened or pitted nails and swollen or stiff joints3. Some people may develop psoriatic arthritis, which affects about 30% of people with psoriasis4.
-
Psoriatic arthritis
PSA is a chronic, inflammatory disease of the joints, where tendons and ligaments connect to bone. No two individuals will experience the condition in the same way. Its severity depends on the individual; some can be affected in multiple places, others may only notice mild symptoms in one or two joints5.
It usually develops 5 -10 years after psoriasis is diagnosed, although some people may have issues with their joints before they notice any skin-related symptoms.
-
Nail psoriasis
Nail psoriasis causes changes to your fingernails and toenails. If you have plaque psoriasis, you may be affected, and so should check for tell-tale signs, such as:
- Tiny dents or pits in your nails
- Discolouration (white, yellow, or brown)
- Crumbling nails
- Nail(s) separating from your fingers or toes
- Build-up beneath your nail
- Blood under your nail
-
When does it develop?
Psoriasis usually develops before the age of 35, affecting men and women equally. It’s particularly prevalent between the late teens and early 30s, and between the ages of 50 and 60.
Genetics play a role in psoriasis and can make some people more susceptible. However, it doesn’t necessarily affect everyone within a family.
-
What triggers psoriasis?
While no one knows the exact cause of psoriasis, scientists believe it’s a combination of things: the immune system causing inflammation, triggering new skin cells to form up to 10x faster than normal13. As mentioned, it can run in families, but can also skip generations.
An outbreak can also be triggered by a number of factors, including:
- Cuts and scrapes
- Surgery
- Medications (e.g. beta-blockers)
- Emotional stress
- Throat infections
- Cold weather
Some factors also increase the risk of someone getting psoriasis, such as having cardiovascular disease and metabolic syndrome or a family history of the condition. If one parent has psoriasis, there’s a 10% chance that their child will go on to develop it. This risk increases to 50% if both parents have psoriasis14.
-
Is psoriasis contagious?
While there’s no known one cause, and the condition has many triggers, psoriasis is not contagious. You cannot ‘catch’ it from being around someone with psoriasis. This includes brushing up against them, swimming in the same water, kissing or having sex15.
Sufferers did not get psoriasis through someone else and can’t infect other people.
-
How to cure psoriasis
There’s currently no cure for psoriasis, however, there are ways to manage the condition and reduce the effect of the symptoms.
-
What makes symptoms worse?
Psoriasis is not caused through poor hygiene, diet or other habits. However, there are certain things that can cause the condition to flare up and worsen. This includes:
- Cold or dry weather
- Stress e.g. an particularly stressful life event, increase in stress levels or chronic stress
- Being overweight or obese
- Smoking
- Alcohol
- Overeating
- Certain medications (e.g. lithium)
- Trauma to the skin
- Hormonal changes
- Infections16
Therefore, a change of lifestyle might be needed in order to reduce the severity of certain symptoms.
-
How to prevent psoriasis
There are some ways to reduce the risk of flare-ups, however, there are no guarantees. These include:
- Showering with lukewarm water, using non-irritating soap and moisturising afterwards
- Wearing loose-fitting, soft clothing
- Eating nutritiously and keeping a healthy diet
- Avoiding smoking17
-
How to treat psoriasis
As mentioned, there’s no cure, but there are ways to make the condition more manageable. Treatments usually come in the form of oils, ointments and creams18, including:
Salicylic acid
Salicylic acid can soften and thin scaly skin, however it shouldn’t be left on for too long, as it can irritate it.
Immunosuppressants
A doctor may prescribe these, they can help as they change how your cells work.
Steroid creams
These slow down immune cells in your skin and can ease swelling or redness. However, they shouldn’t be used on sensitive areas of the skin, such as the face.
Phototherapy
Sunlight can be extremely beneficial for treating skin conditions. Phototherapy involves shining UV rays directly on the skin, as light therapy can slow cell skin growth and ease psoriasis symptoms19.
However, too much exposure to natural sunlight without suncream can increase your risk of skin cancer. 20 minutes a day should be enough.
Natural treatments
Some prefer to use more natural treatments, with options including:
- Salt baths
- Aloe vera
- Apple cider vinegar
- A healthy diet
- Vitamin D supplements
-
Living with psoriasis
Psoriasis can affect your quality of life and how confident you feel. It’s not only visible, which can make sufferers self-conscious, but it can cause pain and irritation, which is both exhausting and annoying. However, there is help out there. Many psoriasis sufferers try different treatments to see what works best for them. Despite this, identifying which treatment is the most effective can be difficult. If you feel a treatment isn’t right for you, or if you have any adverse side effects, talk to a doctor.
The good news is that there’s plenty that can be done to make the condition less painful and difficult to live with.
How can Dermalex help
Dermalex has a range of dermatologically tested skin creams, clinically proven to treat and relieve mild to moderate symptoms of psoriasis. This includes itching, burning, scaled and thickened skin. In fact, 96% of patients saw an improvement in psoriasis symptoms20. Its unique formulation activates the skin’s own repair mechanism to strengthen and restore its barrier, all with a non-greasy finish. Start soothing your skin today!